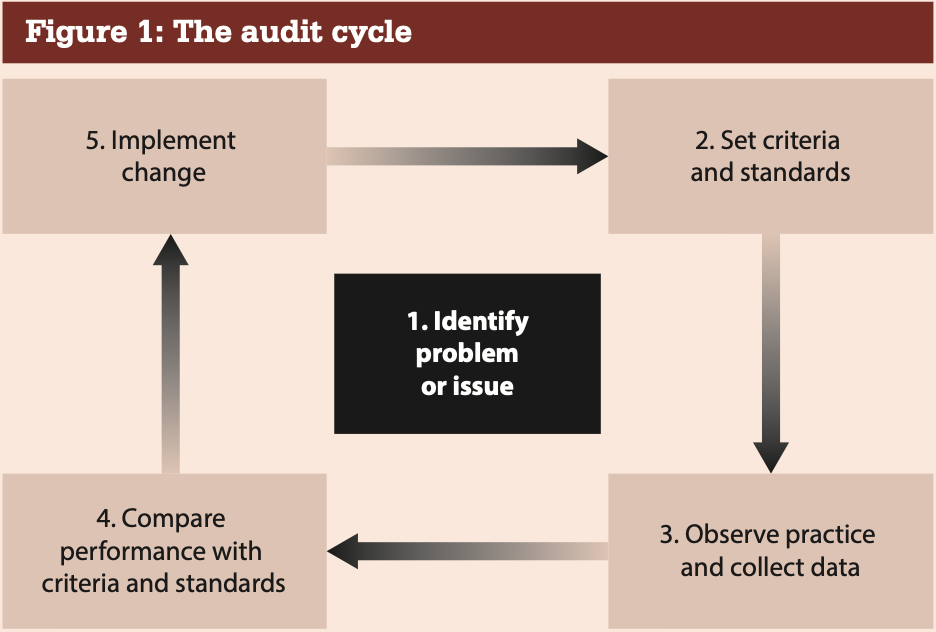
We should be using clinical audit as a continuous cycle of quality improvement, systematically reviewing various aspects of patient care to improve their health outcomes. The reviews are conducted against well described standards and the evidence of documented best practice. Any discovered shortfall should be used to identify the relevant changes necessary to improve future patient care. The process should be repeated at regular intervals to monitor ongoing care. This process is often called the audit cycle (see Figure 1). Audit should be designed with some key principles in mind.
- Identify a clear priority
- Keep it simple
- Keep it focused
- Use measurable criteria
- Conduct the audit over a defined time frame
- LUse audit to support improved practice; this implies completing the cycle: audit is not a one off.
Community pharmacists are required to complete both an annual national audit, decided by NHS England, and an internal pharmacy topic specific to that pharmacy. The 2018/19 audit was on ‘The provision of advice to people with diabetes and advising them on their eligibility to have an annual influenza vaccination.’ Details of this, and other NHS clinical audits for community pharmacy, can be found on the PSNC website.
Have a look at how those audits follow the key principles. Note the 2019/2020 PQS includes, for the first time, a re-audit (on NSAIDs and gastroprotection).
