In OTC
Follow this topic
Bookmark
Record learning outcomes
The word parasite conjures up images of fleas and ticks and other types of troubling bugs that can attach themselves to animals, but in fact a lot of parasitic infections are extremely common in humans. From worms and scabies to headlice, pharmacy teams can reassure customers and support them with over-the-counter (OTC) solutions and self care tips to tackle a range of parasites.
Head lice
Everyone has a head lice story, but despite one in three children getting head lice at some point each year in the UK, many people remain confused about how to detect and treat them.
Community pharmacy staff can play an important role in encouraging parents and carers to keep an eye out for signs of head lice in children, as well as advising on the different treatment options.
“Pharmacy teams should start by reassuring customers that head lice are common as they are easily spread, especially in a school environment, and can be effectively treated with proper measures,” says George Sandhu, deputy pharmacy superintendent at Well Pharmacy. If there is a breakout of head lice among friends or family, George adds: “Advise customers to regularly check behind ears and neck for lice and nits using a fine-toothed comb on wet, conditioned hair every three to four days for two weeks, and avoid head-to-head contact and sharing personal items. In cases of infection use medicated lotions or sprays and re-treat after seven to 10 days.”
If treatment appears to fail, customers should check that the product has evidence of efficacy; they have used enough of it; and it was applied thoroughly and spread through the hair right down to the scalp with a comb. It is also important to check the whole family to guard against the problem of re-infestation.
Threadworms
Threadworms (or pinworms) are a common type of worm infection in the UK, particularly in children under the age of 10. They are tiny, white parasitic worms that infect the large intestine – only of humans – and lay their eggs around an infected person’s anus, usually at night. Along with the eggs, the worm also secretes a mucus that causes itching. If the eggs get stuck on the person’s fingertips when they scratch, they can be transferred to their mouth or onto surfaces and clothes. If other people touch an infected surface, they can then transfer the eggs to their mouth.
Thankfully, threadworms are easily dealt with. “The infection can be treated with a single dose of mebendazole in liquid or tablet form,” says Jacquie Lee, medication safety officer and information pharmacist at Numark. “All household members should be treated at the same time even if they have no symptoms. A second dose two weeks after the first is sometimes needed as the medication kills the worms but not their eggs, which can survive for two weeks.”
Although extremely effective at killing threadworms, mebendazole doesn’t kill their eggs, so there are also hygiene measures that can help prevent a new infection and should be practised for two weeks after treatment. “Most infection comes from inhalation, so regularly washing bedclothes (but not shaking out bedclothes, pyjamas or nightdresses) and performing regular damp-dusting and vacuuming,” adds Jacqui. “Plus ensure children wear close-fitting underwear at night and change it every morning. Everyone should also wash their hands regularly, brush under nails and rinse toothbrushes before use. However, for children under two years of age, or with pregnant or breastfeeding women, pharmacy teams should recommend they consult their GP.”
People should also see their GP if the infection continues two weeks after treatment, as they may need a second dose of medication.
Bedbugs
Bedbugs hit the headlines recently with reports of increasing numbers of infestations across the country. The small insects live in cracks and crevices in and around beds and crawl out at night to bite exposed skin and feed on blood, like mosquitoes.
Although bedbugs can be upsetting to find, pharmacy staff can reassure customers that they aren’t dangerous and don’t transmit any human diseases. Some people develop itchy red bumps after being bitten, which appear in straight lines on the face, neck, hand or arm and can last for several days, but most people don’t develop any serious skin reaction.
However, people should take immediate action to prevent the spread of an infestation, as once in the home, bedbugs are hard to get rid of. The advice from NHS England is for people to contact their local council or a pest control firm, who will use insecticide, a steamer or rapid freeze system to get rid of the bugs.
If people want to tackle the bugs themselves, pharmacy staff can advise them to wash clothes or bed linen at 60°C or put in a dryer on a hot setting for 30 minutes to kill the bugs; dismantle furniture and thoroughly vacuum it, disposing of the contents in a sealed bag; and use insecticide spray specially designed for bedbugs to kill any remaining bugs – but never use this directly on clothing, linen or mattresses.
“Scabies is caused by tiny mites that burrow into the skin”
Scabies
Scabies is caused by tiny mites that burrow into the skin, causing intense itching that’s worse at night, and a skin rash on areas where the mites have burrowed.
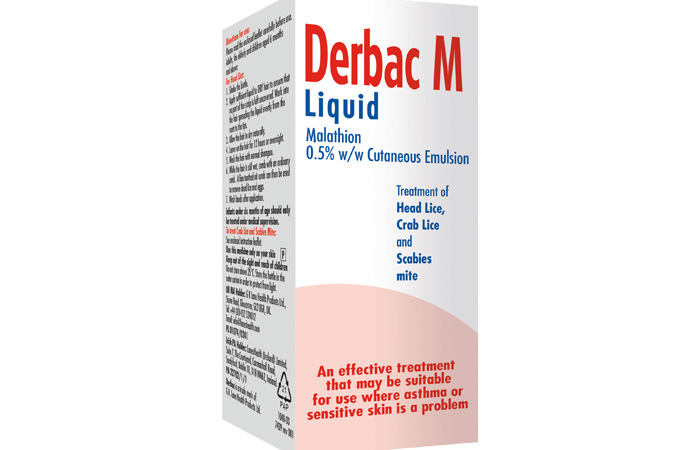
“Scabies is highly contagious through skin-to-skin contact”, warns Samantha Ross, senior product manager for Derbac M malathion treatment for scabies, headlice and pubic lice, “and can lead to more serious complications such as septicaemia, heart disease and kidney problems, so it is important that scabies is treated quickly to prevent its spread”.
When it comes to treatment, Jacquie explains: “Permethrin 5% cream is recommended as the first line treatment and malathion 0.5% lotion can be used if permethrin is ineffective. The treatment needs to be applied to the whole body, including the scalp, if this is affected and left on for eight to 12 hours for permethrin and 24 hours for malathion, before washing it off, ensuring the treatment is applied to areas like between the fingers and toes, wrists, armpits, and buttocks. A second application should be repeated after one week, and a topical corticosteroid can be applied to relieve the itching. All members of the family should be treated even if they have no symptoms, and all bedding and clothes must be washed at 60°C or higher on the first day of treatment (or sealed in a plastic bag for at least 72 hours to allow mites to die). Close physical contact with others should also be avoided until the full treatment course has been completed.”
Having all this knowledge to hand when talking to customers about parasites – and knowing the right products and self care advice to recommend – is vital to help them tackle these unwanted visitors quickly and stop them spreading to other friends and family members.
Market monitor
Product updates from Training Matters
Derbac M is a malathion treatment used to treat scabies, head lice and public lice, says manufacturer G R Lane Health Products Ltd. Available on prescription and in pharmacies throughout the UK, the P line insecticide liquid medicine kills parasites and their eggs – treatment must be repeated seven days post treatment to ensure any remaining lice which may have hatched since first treatment are killed – and is suitable for children and asthma sufferers, adds the company.
G R Lane Health Products Ltd: 01452 52 4012 / laneshealth.com
Common scalp conditions
The scalp’s unique characteristics make it susceptible to a variety of conditions, some of which can lead to hair loss or some type of skin rash.
Dandruff
Dandruff is a common skin condition which causes white or grey flakes of skin to appear on the scalp and in the hair.
Pharmacy teams can reassure customers that dandruff is not harmful and can be simply treated using an anti-dandruff shampoo. There are several different types, but NHS advice is to choose one that contains either zinc pyrithione, salicylic acid, selenium sulphide (or selenium sulfide), ketoconazole or coal tar. Customers should use the shampoo for a month to see if their dandruff gets better, and if not, pharmacy staff can advise them to try again with a different type.
Psoriasis
Psoriasis is a long-term skin condition that affects one in 50 people. It can appear at any age and may come and go throughout the person’s lifetime, affecting the nails and the joints as well as the skin.
Symptoms of psoriasis are dry skin lesions, known as plaques, covered in scales. The plaques can be itchy and/or sore, and normally appear on the elbows, knees, scalp and lower back, but can appear anywhere on the body. In severe cases, the skin around the joints may crack and bleed.
Although psoriasis is a long-term condition, pharmacy teams can reassure customers that there are many effective treatments available to keep it under control.
Topical treatments are usually the first line treatments used for mild to moderate psoriasis and some people find these are all they need to control their condition, although it may take up to six weeks before there’s a noticeable effect. These include emollients which can be applied directly to the skin to reduce water loss and covered with a protective film; and steroid creams or ointments to reduce inflammation, slow the production of skin cells and reduce itching.
Stronger topical corticosteroids can be prescribed by a GP, along with referrals for other treatment options for more serious cases of psoriasis. Pharmacy staff can also remind customers that adopting a healthy lifestyle with a balanced diet, weight management, regular exercise, stopping smoking and reducing alcohol intake might also be helpful.
Hair loss
Hair loss of one form or another is estimated to affect nearly 30 per cent of men before they reach the age of 30, and 50 per cent of males over the age of 50. It also affects many women, and in each case has different causes.
Androgenetic alopecia is the most common form of hair loss in men, but also affects women, and leads to hair loss on the top and sides of the head only. The causes are still not completely understood although, as its name suggests, it is widely thought to involve both hormonal (androgen) and genetic causes.
Female pattern hair loss (FPHL) is also generally genetic and leads to hair loss on the top and sides of the head, due to lowering of oestrogen levels. It is also seen in younger women with Polycystic Ovary Syndrome (PCOS). If this is treated, the hair loss can be reversed.
Traction alopecia is another form of hair loss experienced, most commonly by women, due to physical strain on the follicle from being pulled constantly by tight ponytails, braids and hair extensions. The thinning can be reversible if the problem is identified early, but traction alopecia can cause permanent loss.
Pharmacy staff can advise customers affected by hair loss to see a trichologist for the most appropriate advice. Some people find the over-the-counter (OTC) treatment minoxidil helps to retain the hair they’ve already got – and there are also shampoos that can make hair appear thicker, which can be of some use.
Once again, it is beneficial for pharmacy teams to advise customers about the positive impacts of a well-balanced diet, because without that, hair is unlikely to grow well.
“Psoriasis is a long-term skin condition that affects one in 50 people”
Malaria prevention
Malaria is a serious infection spread by mosquitoes that can be fatal if not
diagnosed and treated quickly. Malaria is found in tropical regions, including:
- Large areas of Africa and Asia
- Central and South America
- Dominican Republic and Haiti
- Parts of the Middle East
- Some Pacific islands.
The World Health Organization (WHO) estimates that there were 249 million malaria cases and 608,000 malaria deaths across 85 countries in 2022. Pharmacy teams can make sure that customers travelling abroad check the malaria risk for the country they are visiting before they go and take steps to prevent infection.
Anti-malarials are not prescribed on the NHS but anti-malaria tablets can be sold under a Patient Group Direction (PGD) and usually need to be taken from a few days, or weeks, before travelling until a few weeks after returning home.
As well as this, pharmacy staff can advise travellers going to areas where malaria is a risk to use 50 per cent DEET-based insect repellent on their skin, sleep under mosquito nets treated with insecticide, and wear long-sleeved clothing and trousers covering arms and legs in the evening, when mosquitos are most active.
As pharmacy teams will often see these people again on their return from holiday, they can also identify anyone who may have contracted malaria and refer them immediately.
The National Travel Health Network & Centre website (travelhealthpro.org.uk) is a useful resource for HCPs and customers alike.