Pharmacists warn ministers at Stormont about impact of NI rises
In News
Follow this topic
Bookmark
Record learning outcomes
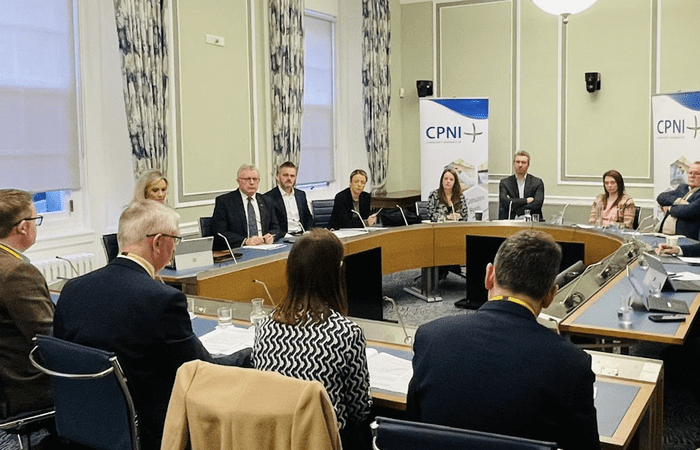
Community pharmacists in Northern Ireland have taken their concerns about the impact national insurance contribution rises will have on their pharmacies to politicians at Stormont.
The pharmacists were joined at the meeting of the All-Party Group on Community Pharmacy by Community Pharmacy Northern Ireland (CPNI) chief executive Gerard Greene, who warned pharmacists were “experiencing unrelenting financial pressures over which they have no control.”
He said national insurance increases would give pharmacists no option but to cut staff numbers or reduce opening hours, jeopardising the health of patients.
National insurance contributions paid by employers will rise from 13.8 per cent to 15 per cent from April 1.
CPNI has estimated national insurance increases, coupled with changes to the national minimum wage, will cost the community pharmacy sector an additional £10 million a year in payroll costs.
“Community Pharmacists are caught in a desperate dilemma: they are clearly demonstrating their value by absorbing pressure on frontline healthcare services,” Greene said.
He added: “On one hand, community pharmacies have been instrumental in tackling winter pressures, with the delivery of flu and Covid and they are testing and treating key health conditions like bacterial sore throats and urinary tract infections, so less patients need a GP appointment.
“On the other hand, they are about to face huge hikes in their running costs when the new national insurance contributions are introduced in April, which they have no way of absorbing.”
The All-Party Group on Community Pharmacy chair Danny Donnelly said: “We all know and value the work done in our communities by community pharmacies providing medications and advice and services to people in need in their local areas.
“We heard about the additional pressures on this vital sector from the UK budget and how this will impact pharmacies across Northern Ireland. We need to see the sector stabilised to fully deliver the services we need to keep people healthy and reduce pressure on other areas of the health service.”