In Clinical
Follow this topic
Bookmark
Record learning outcomes
What we eat is often influenced by circumstances, finances and mood. Before the cost-of-living crisis, people in the UK ate out in restaurants on average 1.5 times a week.
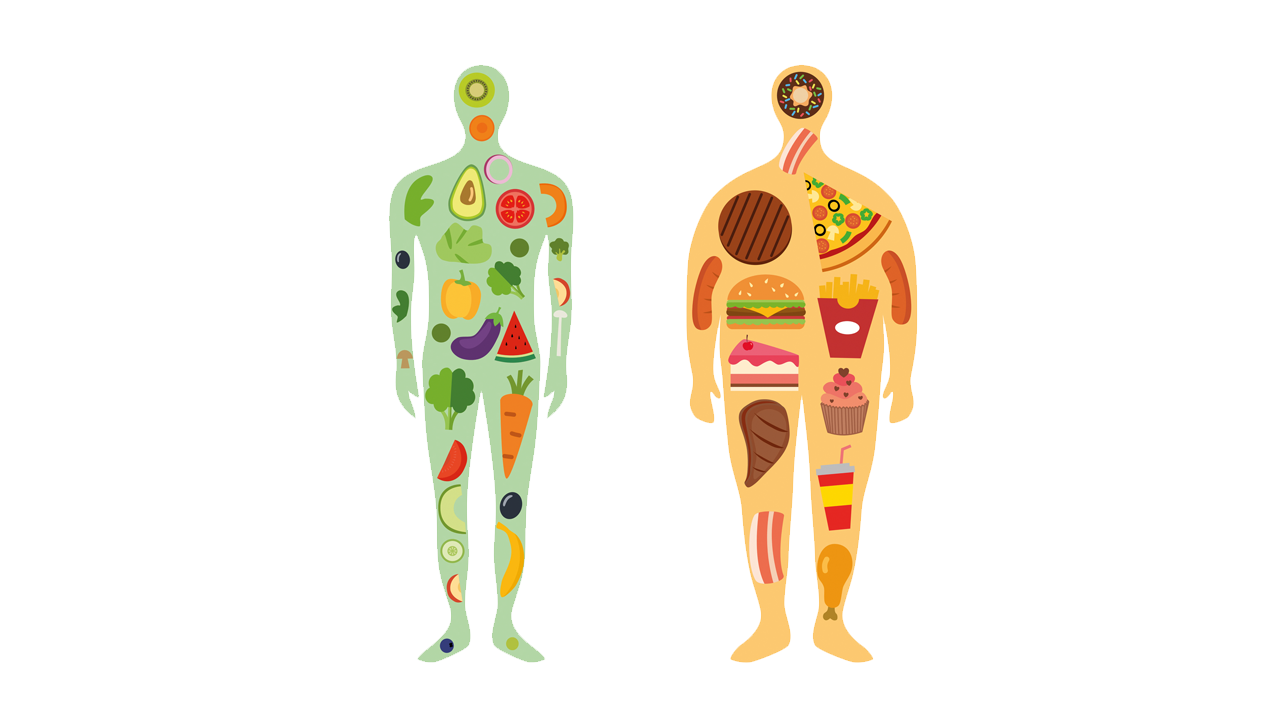
Eating out frequently can mean we are tempted to have a starter and a dessert as well as a main course, and the food can be higher in fat and sugar. In addition, the average consumption of takeaways in the UK is 12 a month with many of these high in fat and calories.
Eating large portions is all too easy, especially when dining with friends or family who may encourage us to eat more than we need. Eating alone, particularly if feeling depressed or suffering low self-esteem, can lead to comfort eating more than needed. Drinking too much alcohol and/or sugary drinks, both of which can contain a lot of calories, also contributes to obesity.
Lack of physical activity is also a factor in gaining weight, but to lose weight requires more than the Government’s recommended 150 minutes a week of moderate intensity activity for overall good health.
Ultra-processed food
A number of studies, including several recent meta-analyses, suggest a relationship between ultra-processed foods and obesity. According to NOVA, a food classification system based on the nature, extent and purpose of the industrial food processing, ultra-processed foods include sweet or savoury packaged snacks, confectionery, packaged bread or buns, industrially reconstituted meat products such as nuggets and their vegan equivalents, and soft drinks.
A 2019 study in BMJ Open found that these foods account for 57 per cent of total energy intake in the UK and 65 per cent of free sugars (all sugar added in any form, all sugars naturally present in juices, purées and pastes, and all sugars in drinks with the exception of dairy-based milk). In the study, 61 per cent of the sample exceeded the recommended limit of 10 per cent of energy from free sugars.
There are several possible reasons for this link. Firstly, ultra-processed food can be very tasty and people who enjoy it like its familiarity. More importantly, perhaps, is the speed at which it can be eaten, with one study showing that participants eating ultra-processed foods consume an extra 17 calories a minute (compared with those consuming unprocessed food), and an average of 500 calories more each day. The higher energy density of ultra-processed food could also help to explain this higher energy consumption.
In the two-week study, participants eating processed foods gained 0.9kg, while those eating unprocessed foods lost 0.9kg. The group eating unprocessed food also had increases in the gut hormone peptide YY (PYY), which suppresses hunger, and leads to decreases in the hunger hormone ghrelin.
The texture of a great deal of ultra-processed food is different to that of unprocessed food and this may make people eat more quickly with the result that the gastrointestinal tract does not have enough time to signal to the brain that the person is full.
Ultra-processed food tends to be high in fat and refined carbohydrate facilitating the consumption of those macronutrients rather than protein. While absolute protein intake may not fall with a diet containing a lot of ultra-processed food, the relative amount of protein as a proportion of energy consumption will.
Protein is the most satiating food macro-nutrient, the mechanism for which is the increase in satiating hormones (e.g. GLP-1, CCK and PYY) that signal to the brain that the person is full. At the same time gut hormones that increase food intake, such as ghrelin, decrease.
Processed snacks and meals are increasingly formulated with additional protein to influence food intake, promote body weight loss and weight maintenance thereafter. Information can be given about the satiating effect of protein with advice to include a source of protein at each meal.
Pharmacological management
Drug treatment should only be used as part of an overall weight management plan. An anti-obesity drug can be considered for those with a body mass index (BMI) of ≥30kg/m2 in whom diet, exercise and behaviour changes have failed to achieve a realistic reduction in weight. In the presence of associated risk factors, it may be appropriate to prescribe an anti-obesity drug to individuals with a BMI of ≥28kg/m2.
Pharmacological interventions should only be used in conjunction with other interventions (e.g. exercise; diet). Since 2010, orlistat (Xenical) has been the only drug recommended specifically for the management of obesity. Orlistat acts by reducing the absorption of dietary fat.
NICE has issued draft guidance on the use of semaglutide in adults with at least one weight-related condition and a BMI of at least 35kg/m2 and, exceptionally, in people with a BMI of 30.0kg/m2 to 34.9kg/m2. Semaglutide can be prescribed only as part of a specialist weight management service for a maximum of two years.
Trial evidence shows that people lose more weight with semaglutide alongside supervised weight loss coaching than with support alone. Patients inject themselves once a week with pens pre-filled with semaglutide. The drug suppresses appetite by mimicking the hormone glucagon-like peptide-1 (GLP-1), which is released after eating. People using it feel full, resulting in them eating less and reducing their overall calorie intake.
Gliptins (dipeptidyl peptidase-4 (DPP-4) inhibitors) are a relatively new class of oral diabetes drugs, usually prescribed for patients who have not responded well to metformin and sulphonylureas or as an alternative to thiazolidinedione medications. Gliptins work by blocking the action of DPP-4, an enzyme which destroys a group of gastrointestinal hormones called incretins.
Incretins help stimulate insulin production when it is needed (e.g. after eating) and reduce the production of glucagon by the liver when it is not needed (e.g. during digestion). They also slow down digestion and decrease appetite. They are effective in lowering blood glucose levels and, because they help reduce appetite, may be beneficial for people needing to lose weight.
Making an intervention
Pharmacy teams are in a good position to talk to patients about obesity to reduce their risk of ill health. The first step when supporting patients to manage their weight is to initiate a conversation.
Research shows that a well-planned brief intervention can increase the chance of a patient making a successful weight loss attempt. Many people will be open to pharmacy teams discussing their weight even if this is not the original reason for their visit. It is important to be aware of obesity services available in the area and also the referral processes. Referral to an obesity service can double the amount of weight lost.
The first stage in a brief intervention is to weigh the patient, measure height and calculate the BMI. It is important to have easy access to weighing scales that are suitable for severe obesity and regularly calibrated. Consideration must be given to the language used in a brief intervention. Examples of useful phrases include: “While you are here, can I check your weight?” or “Before you leave, can I weigh you?”
Consider referral to a weight management service where the patient has a BMI >30kg/m2 or, where there is capacity, a BMI >25kg/m2, particularly where the patient has significant co-morbidities. A commercial weight loss service that accords with NICE guidelines may also be considered if there is no capacity in local NHS obesity services.
When it comes to weight management advice, provide factual information about the risks of overweight/obesity and the benefits of weight loss. Be confident and straightforward in your approach as this will help to build confidence in the patient. He or she will need to make diet and lifestyle changes but it is important not to cast any moral judgements about what people eat.
Ask the patient to fill in a three-day diet diary, including everything they eat and drink, with numbers of spoonfuls, portions, types of bread, cereal, milk and spread, for example, then get them to return to the pharmacy to discuss it. It is usually relatively easy to spot changes that can be made in discussion with the patient.
Suggest a follow-up visit to monitor the patient and provide help and encouragement. You might say something like “I’d like to see how you are getting on so next time you come to the pharmacy I’ll weigh you and we can talk some more”. Follow-up appointments also provide an opportunity to review the patient and encourage them in their weight loss efforts. Ask them what changes they have been able to make and offer to weigh them again.
Give feedback, sensitively but clearly, around an expected weight loss target of 1kg each week. Review the proposed action for weight loss and any further changes the patient feels they can make. Some patients may not be willing to commit to losing weight straight away or being referred to a weight loss service. If this is the case, acknowledge how hard it can be to lose weight and tell them you will be there to support them when they feel ready to tackle their weight.