Which symptoms are involved?
Our understanding of ongoing symptoms comes from a range of research studies including large- scale surveys and in-depth qualitative research to explore the patient experience in detail. The most common symptoms are fatigue and breathlessness but a large range of other symptoms is also recognised and the list has been growing.
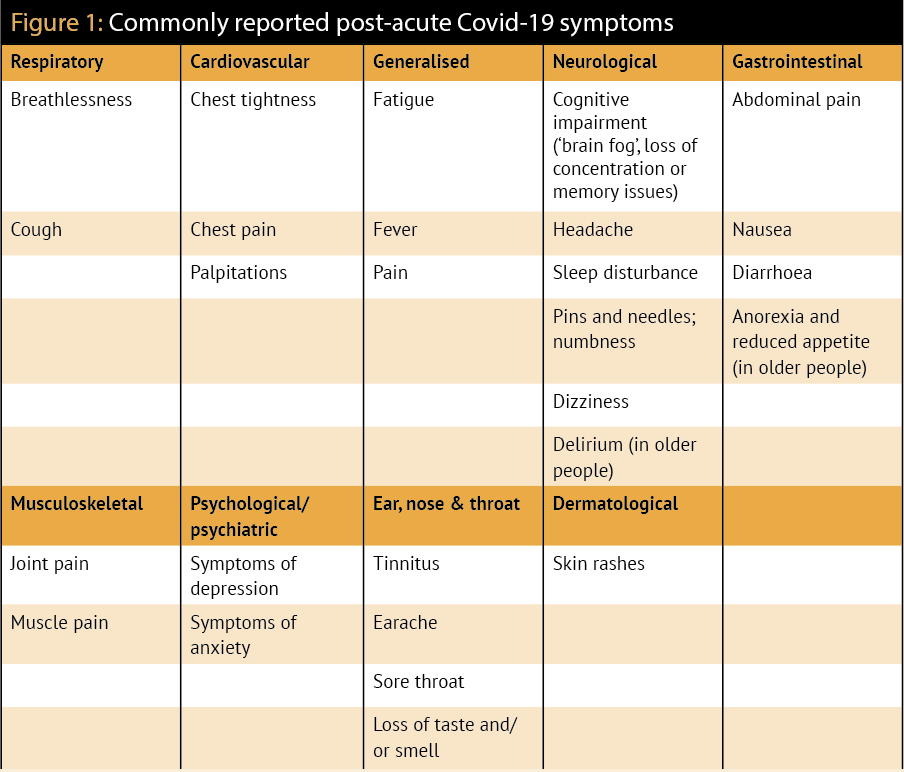
An editorial in the BMJ recently (April 2021) listed fatigue, cognitive dysfunction, wheeze, inappropriate tachycardia and gastrointestinal disturbance as frequently reported symptoms of long Covid. The main symptoms reported in the NICE guideline are shown in Figure 1.
Quantitative data cannot tell us how it feels to be a patient with ongoing Covid-19 symptoms. This is where qualitative research can shed some light. Patients have described multiple, unpredictable symptoms, which sometimes fluctuated over time. Some often have periods
of relative wellness before relapses.
One patient reported being “fatigued to the point of having to sleep in the day, inability to exercise, continued shortness of breath both motionless and when exerting, small waves of anxiety, considerable depression, continued loss of smell”. Also “brain fog” is commonly reported and its effects can be debilitating, with difficulties in focusing and concentrating, and experiencing headaches.
Listening carefully to patients is an important part of tackling potential biases against long Covid, and also inequality in access to healthcare and subsequent differences in health outcomes. Asking about the nature, severity, timing and duration of symptoms will help your decision-making.
It is also useful to understand what experience a patient has had with acute symptoms and the severity of their condition. For instance, did they require a stay in hospital? Did this prove to be a traumatic experience?