Atopic eczema is believed to result from a gene-environment interaction.2 Genetic factors lead
to a weakened skin barrier, which can easily be damaged by a range of environmental factors including irritants, such as harsh detergents and abrasive clothing, allergens (e.g. animal dander, house dust mites, moulds and pollens) and other factors (e.g. changes in humidity, psychological stress). Food hypersensitivity plays a role in a small number of children under the age of three years.
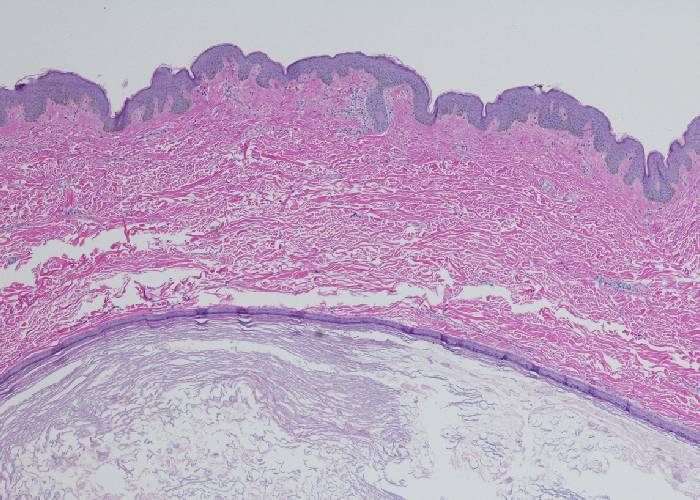
The skin barrier describes the way that the stratum corneum operates to keep irritants and allergens outside and water inside the skin. It is often envisaged as a brick wall where skin cells (corneocytes) are the bricks and lipid bilayers make up the mortar. Anything that disrupts this orderly structure, such as detergents that remove skin lipids, impairs the barrier function leading to water loss from the skin cells.
Water inside skin cells keeps the skin pliable, springy and smooth. Water loss leads to roughness and cracking of skin and weakening of the barrier so that allergens and microbes can penetrate.
Natural moisturising factor (NMF) – a mixture of humectant substances including urea, sodium pyrrolidone carboxylate, lactic acid and others – helps to hold water in skin cells. The skin lipids comprise fatty acids, cholesterol and ceramides.2
The skin barrier is least robust in areas where the skin is thinnest, such as skin creases and on eyelids. The skin barrier is relatively fragile at birth and increases steadily in strength during the first few months of life. Eczema often appears first in areas where the skin is thinnest.
A flare-up of eczema typically starts off as red, itchy, inflamed, sore areas of skin – often on the inner side of elbows or wrists, or behind the knees. Chronic eczema tends to be areas of thickened, dry, cracked skin that has been repeatedly scratched or rubbed. Small patches of broken skin are common because of frequent scratching.
