In OTC
Follow this topic
Bookmark
Record learning outcomes
The average woman menstruates for over 34 years, with most starting at the age of 12 and continuing to have periods every month up until the average age of the menopause, which is around 51 years old.
Menstruation can bring with it a whole host of issues, from fluctuating hormones to stomach cramps, and while many women experience trouble-free periods, for those who don’t, there can possibly be something more severe at play.
Dysmenorrhea
Dysmenorrhoea (painful periods) is painful cramping that occurs in the abdomen before and during menstruation, with signs and symptoms including pain radiating to the lower back or thighs, nausea, headaches, dizziness, and fatigue.
“There are two forms of dysmenorrhoea,” explains public health nutritionist and spokesperson for reproductive health supplement Kaneka Ubiquinol Co-Enzyme Q10, Emma Derbyshire. “Primary dysmenorrhea begins around six to 12 months after menstrual cycles begin, so it is with women and girls from the start. Secondary dysmenorrhea tends to start later in life even after years of painless periods, and can be caused by underlying conditions such as fibroids, polyps, pelvic inflammatory disease or endometriosis.”
Thankfully there are plenty of over-the-counter (OTC) and self care options that pharmacy teams can advise customers experiencing painful periods to try.
“Patients can consider OTC pain relief like ibuprofen and paracetamol and using heat therapy (hot water bottles or heat patches) to relieve some of the painful symptoms,” says Jacquie Lee, Numark medication safety officer and information pharmacist. “It is worth discussing hormonal contraception as this will reduce many of the symptoms. However, patients should be advised to see their GP if pain is severe, worsens over time, or affects daily life.”
For those who favour vitamins, minerals and supplements (VMS) as a first-line treatment option, Emma says: “A recent meta-analysis of six randomised controlled trials showed that zinc supplementation (a dose as low as 7mg/d) helped to achieve pain relief in women with primary dysmenorrhea. Zinc is also found in foods such as fish, seafood and meat, beans, nuts and seeds.”
“Pro-inflammatory diets have been found to increase endometriosis risk”
Endometriosis
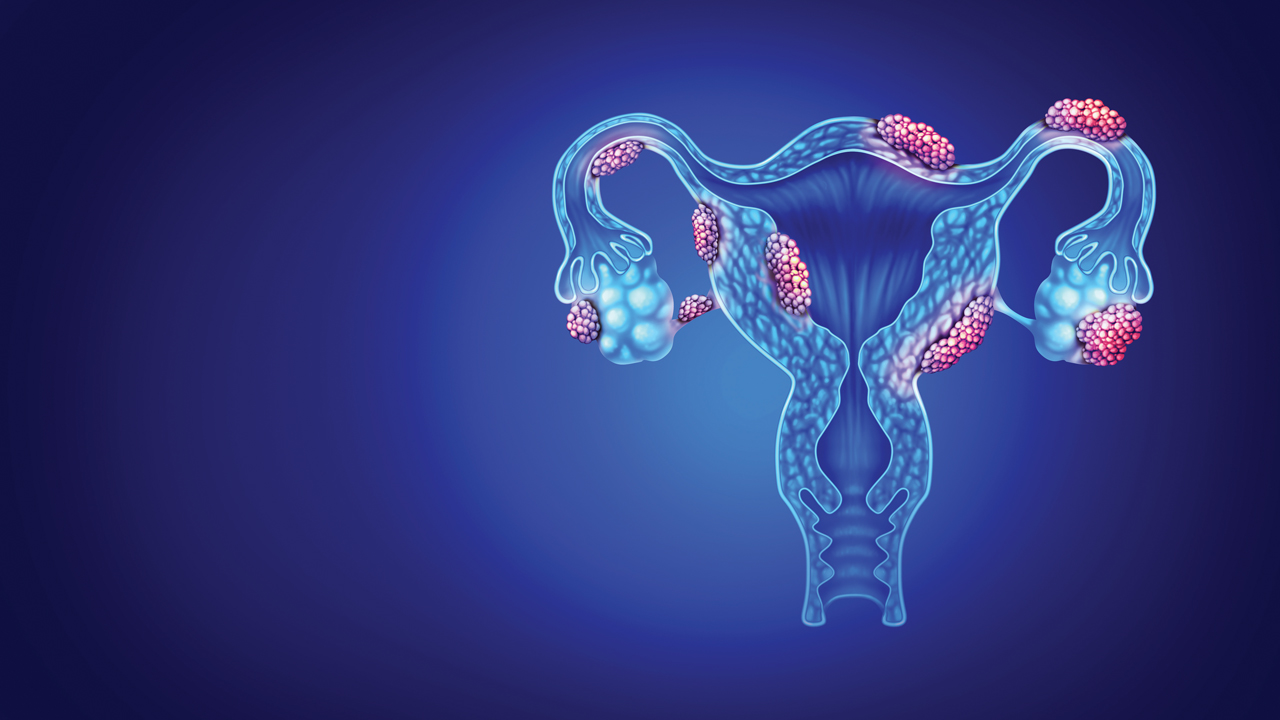
Endometriosis occurs when cells like those lining the womb grow in other parts of the body such as the fallopian tubes, ovaries or lining of the pelvis.
Symptoms of endometriosis can include heavy or irregular periods, severe pelvic pain (especially before/during menstruation), heavy periods, pain in the lower tummy and back, fatigue, bloating, pain during or after intercourse, painful bowel movements or urination (worse during periods), and even difficulty conceiving. In addition, people with endometriosis may also experience anxiety or low mood.
“Patients can consider OTC pain relief like ibuprofen and using heat therapy as an adjunct to relieve some of the painful symptoms”, says Jacquie, “and staff could suggest keeping a symptom diary for tracking patterns, as they are often related to menstrual cycles. Patients can also be signposted to their GP for further investigations which may include ultrasound and laparoscopy”.
Some people find relief by making some dietary changes. “Pro-inflammatory diets, such as those providing a high intake of sugar, highly processed foods high in trans fatty acids, and saturated fat intake have been found to increase endometriosis risk,” says Emma. And, when it comes to supplementation, Emma adds: “Some research with young girls (12-25 years) showed that taking fish oil (1000mg) over six months helped with pain reduction, but more research is needed to replicate findings and unravel why.”
There may be some good news for endometriosis sufferers from The National Institute for Health and Care Excellence (NICE), which has recently recommended the first daily pill to treat endometriosis in England and Wales. Final draft guidance published in March 2025 saw NICE approve the relugolix combination therapy or Ryeqo (Gedeon Richter) pill, which it estimates could benefit around 1,000 women each year. The treatment can be taken at home, starts working more quickly than injectable treatments and combines all required hormones in one pill.

Using heat patches or hot water bottles is one of the best ways to soothe period pains.
Adenomyosis
Adenomyosis is an extremely painful and debilitating condition where the lining of the uterus starts growing into the muscle in the wall of the womb.
Most common in women over the age of 30 years, symptoms can include heavy bleeding and prolonged, painful periods; an enlarged or tender uterus (which may cause a bloated feeling); pain during intercourse; and chronic pelvic pain.
“Again, pharmacy staff can recommend pain relief such as ibuprofen and paracetamol, and suggest that the patient keeps a menstrual diary to monitor symptoms,” says Jacquie.
Patients may need to be signposted to their GP for an ultrasound to diagnose the condition, with treatment options including hormonal therapy, and surgery – including hysterectomy – in severe cases.
Dietary considerations that may help with the symptoms, according to Emma, include “eating fruit and vegetables full of antioxidants which have anti-inflammatory effects, and eating oily fish such as salmon, mackerel, sardines and trout for their anti-inflammatory effects generated through the omega-3 fatty acid metabolic pathway”.
Tackling period poverty
Period poverty is when someone can’t afford the menstrual products they need in order to manage their periods safely and with dignity. This can make periods a monthly struggle, especially for people on low incomes or experiencing homelessness.
Action Aid estimates that 2.8 million people in the UK can’t afford period products – which equates to one in five people who menstruate – causing some to miss school or work, or to use unsuitable alternatives like toilet paper, socks or even newspaper.
Several UK-based organisations are campaigning to end period poverty and promote menstrual equity:
- Freedom4Girls – Supports people in the UK and globally, offering education and distributing free period products
- Bloody Good Period – Provides menstrual supplies to those who can’t afford them, especially asylum seekers, refugees and those in precarious living situations
- Period Poverty UK – Focuses on campaigning and awareness to ensure that no one misses out on education or work because of their period
- The Hygiene Bank – Distributes hygiene products, including period products, to people in need via a national network of community partners.
As trusted, accessible spaces, community pharmacies are ideal places to help address period poverty in local communities. Here’s how pharmacy teams can get involved:
1. Stock affordable, inclusive options
Make sure your pharmacy offers a range of branded and unbranded period products from pads and tampons to reusable options, at different price points.
2. Donate or partner with local initiatives
If your pharmacy has the capacity, collect donations of menstrual products to pass on to local schools, food banks or charities, or become a drop-off point for groups like The Hygiene Bank.
3. Educate and raise awareness
Talk about period poverty with colleagues and customers when appropriate, and support campaigns that raise awareness.
4. Signpost to support organisations
Let customers know about local and national organisations offering free products and support. Keep leaflets or posters in-store or include links on your pharmacy website or social media.
Polycystic Ovary Syndrome (PCOS)
The main features of polycystic ovary syndrome include irregular periods, as the condition means the ovaries are not ovulating regularly. People with PCOS may also have surplus androgens – hormones that fuel the growth of excess facial and body hair (also known as hirsutism) – and ovaries that are enlarged and contain fluid-filled sacs but do not contain cysts, despite the name PCOS.
Other symptoms can include thinning of the hair, oily skin, acne, weight gain – particularly around the abdomen – and difficulty conceiving. People may also experience insulin resistance symptoms such as skin darkening and sugar cravings.
“Advice to offer patients includes encouraging them to maintain a healthy weight through diet and exercise, and in some cases they may be able to access weight management services. Staff can also discuss blood sugar management by eating a low-GI diet and having regular meals,” says Jacquie.
“There are also suitable OTC treatments for acne or excess hair growth that may be appropriate, and of course patients can be signposted to their GP for diagnosis and potential treatment including hormonal contraceptives and metformin.”
Lifestyle considerations may also be useful. “Consuming antioxidant rich foods such as berries, citrus foods or drinking herbal teas may help to counteract inflammation,” says Emma. “The Mediterranean diet and omega-3 rich diets have also been found to be beneficial for PCOS. There is some emerging evidence that probiotics (live microorganisms), prebiotics (foods that encourage microbiota establishment), and synbiotics (combinations of pro and prebiotics) could help to improve the microbiome, which is generally altered in PCOS women but, again, more research is needed to study this in depth.”

Women experiencing severe pain should be referred to the GP for assessment.
“Action Aid estimates that 2.8 million people in the UK can’t afford period products”
Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease is when the female reproductive system has an infection in the ovaries, fallopian tubes and/or womb.
Symptoms of PID can include lower abdominal/pelvic pain, pain during sex or urination, bleeding between periods or after sex, heavy and/or painful periods or spotting, vaginal discharge that may be yellow or green and have a pungent odour, and fever and fatigue.
“Patients should be advised to immediately see their GP or sexual health clinic for testing and antibiotics,” says Jacquie. “In the meantime, they can be advised about safe sex practices including using condoms and sexually transmitted infection (STI) screening.”
While nutrition on its own won’t tackle an infection or an STI, Pamela Mason, nutritionist from the Health and Food Supplements Information Service (HSIS), says: “Eating foods and consuming drinks rich in antioxidants such as blueberries, dark chocolate, beans, black and green tea or taking a multivitamin and mineral supplement formulation that includes antioxidants such as vitamin A, C or E may help to attenuate oxidative stress and improve the function of the immune system, which may help with PID management.”
Pharmacy teams are the instantly available face of professional healthcare advice, making them ideally placed to provide information and support to customers with menstrual problems, and break down the taboos that often surround this sensitive issue.
Incontinence in women
There are several types of incontinence in women that can be differentiated by their signs and symptoms.
Stress incontinence shows as leaking urine during activities (laughing, coughing, exercise), whereas urge incontinence shows as a sudden, urgent need to urinate. Other symptoms include frequent urination, nighttime waking and difficulty emptying the bladder completely.
“There are various ways pharmacy staff can provide support to women experiencing incontinence,” says Jacquie Lee, Numark medication safety officer and information pharmacist. “They can recommend incontinence pads or liners for symptom management, discuss lifestyle adjustments that may reduce episodes (reducing caffeine/alcohol, maintaining hydration), and suggest exercises and bladder training which can be beneficial, such as Kegel exercises and timed voiding techniques.”
Bladder weakness can also accompany menopause as estrogen levels start to fall, and pelvic floor muscles weaken, commonly leading to stress urinary incontinence and an overactive bladder.
Once again, pelvic floor exercises can help with muscle control, and customers can also talk to their GP about medication or further referrals for other treatment options. Hormone replacement therapy (HRT) can help, and pharmacy teams can encourage women to talk to their GP about the benefits and risks.
In the meantime, pharmacy staff can recommend a wide range of discreet incontinence products which are more appropriate than the sanitary pads some women choose to use, but which don’t work as well for incontinence.
The benefit of squats
Finding time for exercise can feel like another item on an already overwhelming to-do list, but Amanda Olson, president and chief clinical officer at women’s health products company Intimate Rose, says daily squats are one of the most effective exercises women can do to improve pelvic floor strength, prevent incontinence, and enhance bone density while also boosting circulation and mental health.
While squats are accessible to most women, Amanda says proper form is essential to maximise benefits and prevent injury: “Stand with feet hip-width apart or slightly wider. As you lower your body, push your hips back as if sitting in a chair. Keep your chest up, back straight, and ensure your knees track in line with your toes without pushing forward past them,” she explains. “Most importantly, engage your core throughout the movement and exhale as you rise.”